Two of my good friends are 45 years old and both separately speak of being in perimenopause. One is experiencing unexplained anxiety and depression, which she can only attribute to menopause. And my other friend swears she’s going through perimenopause due to well-documented symptoms including fatigue, loss of sex drive, and irregular periods.
They both seem convinced, and I’m impressed because perimenopause is somewhat of a mystery to me even though I’m 50. It also goes to show how women experience the menopause transition or ‘the change’, as it’s also called, differently.
At the age of 45, I was potty training my 3-year-old and settling my 5-year-old into kindergarten, and I hadn’t even heard of the word perimenopause, let alone considered I might be in it. And then, Boom! Debilitating hormonal migraines took hold with gripping force and settled into a monthly occurrence in my life.
At that point though my life revolved 100% around my kids’ needs and I couldn’t muster up the energy or self-focus to work out that my piercing migraines were possibly linked to menopause. My doctor and then neurologist confirmed it, though. And they’ve only got worse over the years.
In a nutshell, perimenopause is the transition from when your levels of estrogen (the main hormone in women) start decreasing, to the point where they finally cause your ovaries to stop releasing eggs. When you’ve gone 12 months with no period, it should then completely stop and you will officially be in menopause.
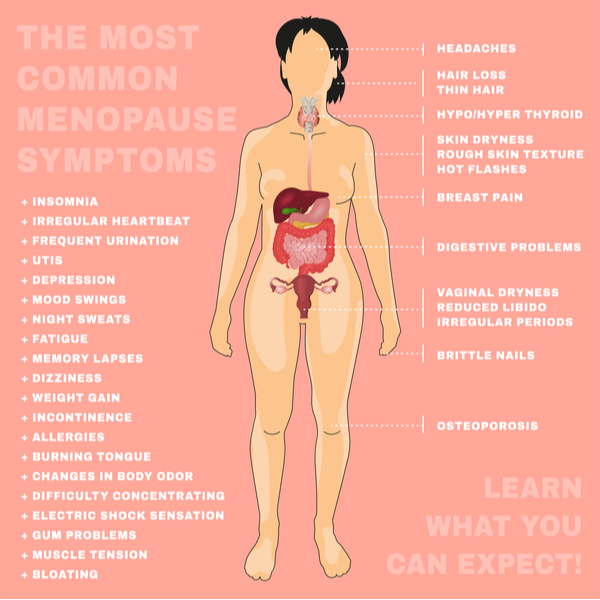
There are a whopping 34 documented symptoms of perimenopause (see pic below). Yes, after having periods for years and many of us then going through childbirth, we definitely don’t get off lightly as our reproductive system winds down.
According to the North American Menopause Society, perimenopause can last to 4-8 years, while the National Institute on Aging says it can last from 7-14 years, which won’t give any of us much comfort!
For the lucky though, it can last just months. And if you’ve ever wondered why its perimenopause and not premenopause, it’s because premenopause is when you have no obvious signs of symptoms (although you may or may not experience irregular bleeding), while perimenopause is when you do have symptoms.
So, we know what perimenopause is, but how do we really know we are in it? I spoke with Dr Kathryn Macaulay, Professor of Obstetrics, Gynecology, and Reproductive Sciences at UC San Diego Health, to get the details.
*The following answers are for general information purposes only. They are not for a specific diagnosis. Speak to your own doctor if you are experiencing any of the symptoms in this article.
Please sum up how you know you may be in perimenopause.
The first way to know you’re in perimenopause is if you’re 45 years or older [unless you have early onset] and you start to notice a change in your menstrual cycle length. The cycle is from the first day of one period to the first day of your next period, and a warning sign is if you have more than a seven-day difference from the first day. If the number of those days starts to differ – especially if you’ve usually had regular periods – like if you’re having 45 or 60-day cycles, that is often one of the earliest indications that perimenopause is starting.
Sometimes hot flashes, or nocturnal hot flashes (also known as night sweats), are also hallmark symptoms of perimenopause, and 75-85% of women experience them to some degree. They can sometimes start when periods are still regular, but generally it’s accepted that the change in your menstrual cycle is when perimenopause is starting.
Do some women experience more frequent bleeding during perimenopause also? If so, why, and how much should be cause for concern?
Yes. Women can sometimes have too much bleeding in perimenopause due to changes in the ovary not ovulating consistently every month. They can have abnormal bleeding less than 21 days apart, or they can have excessively heavy flow lasting more than 7-8 days. But usually the typical pattern for perimenopause is to start having longer number of days between periods (a.k.a. menses), e.g. skipping periods.
Is there a blood test to check for perimenopause?
Yes, the blood test includes testing the follicle-stimulating hormone (FSH) and estradiol, which is the predominant estrogen hormone in a woman’s blood circulation. But blood work isn’t always helpful as the level of hormones can fluctuate quite a bit. There can be times when estrogen is low, and times when it can be higher than usual, which is normal between ages 45-55. When I see a patient’s hormone test result, my first question is ‘what’s going on with your menstrual periods’, because that’s really how you diagnose perimenopause.
So the blood test isn’t a definite sign?
The problem is that perimenopause can look just like menopause is setting in and then 4-6 weeks later it can look like you’re cycling more normally again. So you can’t use the blood test to predict that someone is in menopause. Entering perimenopause isn’t a lab definition, it’s a clinical definition. Women really have to be tracking their own periods.
What’s going on with our hormones during this time?
Fluctuation in hormones can be particularly tricky for women in perimenopause, in terms of causing mood disorders, depression and anxiety, or migraines. The ovaries are kind of sputtering out. They’re still producing hormones but they can be erratic. And it can go on for a few years, so it can be a tricky time for women to navigate with hot flashes starting and/or mood changes. There are different approaches to help women through the different symptoms.
What advice do you give women experiencing hot flashes or night sweats? Can they take any medication to help ease them?
Estradiol (hormone therapy) is most effective treatment for hot flashes and/or night sweats but there are certain non-hormonal treatments that can work as well.
A friend who suffered from terrible perimenopausal migraines was told by her doctor that it meant that she probably wouldn’t get hot flashes. That you get one or the other. Is that true? Please say yes!
Sorry, that’s not true at all. They’re different processes in the brain and are triggered differently by estrogen.
Why are migraines a symptom of perimenopause?
There’s a thought that it could be fluctuating hormone levels that exacerbates symptoms. It’s not necessarily that perimenopause causes migraines but more that women who are prone to migraines may have a worsening of the symptoms at that time. A new onset of migraines can happen during perimenopause but is more unusual.
How do you treat women with perimenopausal migraines?
Sometimes we put women in that age group who don’t experience migraine with aura, or who don’t smoke, on a low dose birth control pill that they take continuously so they have no drop in hormone. That can work for some women. You don’t ovulate and it quiets the ovaries down so that the birth control pill becomes the steady hormone.
Does having a baby later in life delay perimenopause?
No.
When is it dangerous to blame perimenopause?
If you’re having abnormal bleeding, or pain with intercourse or urination, don’t just blame hormones. That’s done way too much. Your reader’s story is an example. It could be hormonal but if there’s something that’s perceived as a problem, get it evaluated and don’t ignore it. People really stretch out blaming hormones over too many things. We’re told, ‘You’re a woman, therefore it’s a hormonal thing’, and that’s just not appropriate. I hear a lot of that.
Does perimenopause affect your cholesterol levels and potentially cause vitamin deficiencies?
There is no direct effect on lipids or vitamin deficiencies from perimenopause that I am aware of, although I do recommend increasing dietary calcium and vitamin D supplementation once you’ve reached menopause, for osteoporosis prevention.
Many symptoms are similar to things we experience getting older – like memory loss and brain fog – does that mean they can get better after we experience menopause?
During perimenopause, memory loss and/or brain fog can be worse but then once one has reached menopause and hormone levels are no longer fluctuating, cognitive complaints typically improve.
Are being ‘in’ menopause and being postmenopausal the same thing? The labels get confusing.
Perimenopause refers to the menopause transition, and one has reached menopause when they have had 12 consecutive months without a period. After that we say they are postmenopausal.
If women experience other symptoms like insomnia, anxiety, or depression, do you refer them to other specialists?
Yes. If women have persistent insomnia, depression or anxiety then I refer them first back to their primary care doctor, or possibly a specialist. Especially if they already take hormone therapy and things are not improved.
Can women gain more weight more easily during perimenopause?
Yes. I do a lot of weight counselling for women in their 40s who are overweight, and I really encourage them to use the time during perimenopause to try to lose weight. The healthiest thing you can do entering the menopause is to enter into it at a normal weight range. I recommend patients do all they can do in their 40s before menopause to get back to their ideal body weight, or at least in a healthy BMI range. Why? For cancer risk, cardiovascular risk, and diabetes risk. Some women find it’s more difficult to lose weight after menopause, so eat healthily and exercise regularly during perimenopause. Enter into menopause at a healthy weight and you’ll be way ahead of the game.
Any good news?!
Yes! When you finally reach menopause, you’re free from periods and PMS symptoms, and you don’t have to worry about contraception so there’s some freedom with that. Also, the majority of menstrual-related triggered migraines do seem to improve. Even in general, other kinds of migraines tend to improve after menopause. It can be a little tricky if you’re taking estrogen therapy for hot flashes because estrogen has a role as a trigger for migraines, but discuss this with your doctor. It’s also a great time for women to do a proper health assessment. Are you your ideal weight? Check you’re taking enough vitamin D and check your cardiovascular health.
I try to focus on the positive for my patients. Menopause for a lot of women is not necessarily a disruptive health transition and when it’s natural spontaneous menopause it’s a natural part of the reproductive life span. It gets a really bad rap that’s kind of sexist, like the hormones and mood changes. Patients say, ‘I’m irritable and my husband said I should come see you’. I try to steer away from depicting it like that. It doesn’t need to be viewed as a medical disease or disorder.
Dr. Katherine Macaulay is a Professor of Obstetrics, Gynecology, and Reproductive Sciences at UC San Diego School of Medicine, where she also heads up the Menopause Health Program.